I began to wonder what we were missing as psychiatrists: were there other approaches that would better serve our patients?
In an effort to help more patients, I spent the last fifteen years studying and evaluating new approaches for mental health conditions. The most useful framework I found is functional medicine psychiatry, an approach that identifies and addresses underlying factors that contribute to brain-based conditions.
Before looking at functional medicine psychiatry, let’s look more closely at the limitations of the current model of psychiatry and why there is a need for a better approach.
Why Standard Psychiatry Sometimes Falls Short
A recent study in the American Journal of Physical Anthropology found that despite the increased use of antidepressants and other conventional treatments, the global prevalence of both depression and anxiety remained essentially the same between 1990 and 2010.
In other words, the rates of these disorders are not improving, and people aren’t getting better.
Data provided by the Center of Disease Control and Prevention (1) (2)
Why are psychiatric outcomes lagging behind those in other medical fields? This is, in large part, because of a diagnostic framework that focuses on symptoms without considering underlying disease.
Symptoms Don’t Tell the Whole Story
When it comes to diagnosing patients, psychiatrists use a manual called the DSM-V that classifies mental disorders based on clinical symptoms. While the DSM-V has been helpful in creating a common language for practitioners and patients, the diagnoses are not based on any true understanding of the brain’s biology or the diseases and disorders that affect it.
The former head of the NIMH stated in a 2013 letter that, “Unlike our definitions of ischemic heart disease, lymphoma, or AIDS, the DSM diagnoses are based on a consensus about clusters of clinical symptoms, not any objective laboratory measure.” He says that other areas of medicine have replaced this symptom-based diagnosis, as we have learned that “symptoms alone rarely indicate the best choice of treatment.” Psychiatry, however, has yet to move on from this symptom-based approach.
He then announced that the institute would not fund any research based on DSM-V diagnoses, citing the need for new and better treatments.
Because our diagnostic criteria don’t capture the true underlying disorders, it’s no surprise that current medications don’t work for some patients.
SSRIs: Are They Effective?
The most commonly prescribed medications are SSRIs. When they were introduced in the 1990s, psychiatrists believed we had entered a new era with medications that were more effective, had minimal side effects, and should be easy to get off of with few withdrawal symptoms.
However, a number of comprehensive studies have revealed that even though SSRIs are effective for some patients, they are less effective than we previously thought.
Two larger scale studies found that:
-
Roughly 20 to 40 people out of 100 experienced improvement after taking a placebo
-
Roughly 40 to 60 people out of 100 experienced improvement after taking an antidepressant
That is, the antidepressant only helped an extra 20 out of 100 people.
Many psychiatric medications, including SSRIs / SNRIs, mood stabilizers, and antipsychotics, are based on the chemical imbalance theory, which argues that a lack of serotonin and other neurotransmitters causes anxiety and depression. But the picture is much more complex than that. In reality, these disorders involve many more root causes than just neurotransmitter levels in the brain.
As for withdrawal symptoms, patients have reported experiencing nausea, irritability, insomnia, confusion, and fatigue when tapering off SSRI medications.
Though these medications play an important role in psychiatric treatment, they are not the magic bullet we had hoped they were. In order to develop more effective treatments, we need to identify the root cause of psychiatric symptoms, which is the approach taken by functional medicine.
What is Functional Medicine Psychiatry?

Functional medicine psychiatry is an evidence-based approach that helps us understand root causes of brain dysfunction through laboratory testing and, when needed, brain mapping.
In every other field of medicine, doctors search for the underlying cause of symptoms with imaging and testing. It’s time to take this diligent approach with psychiatry.
Of course, not all root causes are biological and based on laboratory results. In addition to biological contributors, trauma, adverse childhood events, current stressors, and cultural factors can all impact emotional and behavioral health and should be taken into consideration.
Current PRACTICES OF Psychiatry
-
Symptom-based approach
-
Treatments based on neurotransmitter research
-
Testing rarely used and based on standard reference ranges
-
Generic treatments for diagnoses
-
Focuses on chemical imbalances in the brain
-
DSM-V largely ignores psychosocial factors
Functional Medicine Psychiatry
-
Root cause approach
-
Treatment based on broad up-to-date research
-
Comprehensive and sensitive testing with defined ranges for optimal health
-
Individualized treatments for patients
-
Considers the brain in context of whole body health
-
Considers psychosocial factors
How can functional medicine psychiatry identify the underlying biological causes of my symptoms?
1. Cutting-Edge Research
While conventional psychiatry focuses only on neurotransmitter imbalances, functional medicine psychiatry looks more broadly at the most up-to-date research on diagnostic techniques and factors that affect brain health.
One example is brain mapping, or quantitative EEG, which involves taking a patient’s brainwave activity and comparing it to a database of healthy people. This brain map allows us to see areas of brainwave activity that may be under or overactive. For instance, patients with anxiety tend to have too many stimulating beta waves and not enough relaxing alpha waves.
Research in recent years has also shown the impact of systems outside the brain on psychiatric and emotional health. The GI tract is a perfect example. We know that the gut microbiome influences the stress response and contributes to anxiety and depressive behaviors, and that dietary habits influence the health of the microbiome. Yet few psychiatrists ask patients about their diet or gut-related symptoms.
2. Comprehensive and Sensitive Testing
Testing is rarely done in standard psychiatry, and the few tests that are ordered usually fail to show anything significant. In fact, many patients with psychiatric conditions have been told that their labs are normal, even though they continue to experience symptoms.
Functional medicine uses testing in two important ways:
-
Tests are broader and more comprehensive to identify key factors that tend to be overlooked, such as mineral deficiencies, inflammation markers, and chronic infections.
-
Tests use optimal ranges for significant findings.
-
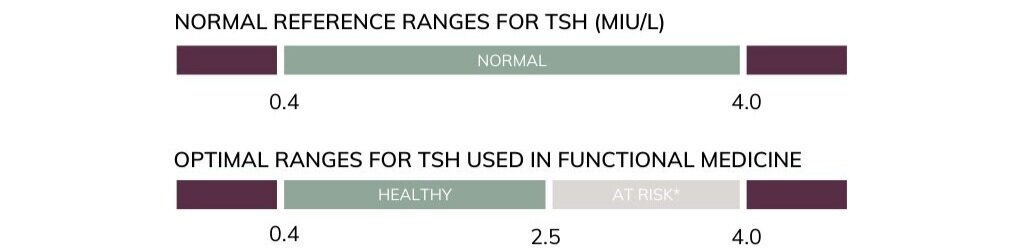
Conventional doctors use reference ranges that are based on population norms, which show average levels but not healthy functioning in patients. By contrast, functional medicine practitioners use more defined ranges that correlate with optimal health.
-
For example, patients who have a thyroid-stimulating hormone level (TSH) between 2.5 – 4.0 mIU/L are more likely to suffer from depression* and benefit from treatment, despite the fact that they fall within the “normal range.”
-
3. Whole Body Health
Studies show that the brain is interconnected with other parts of the body, especially the immune, GI, and endocrine systems. A functional medicine approach argues that brain health and function can only be understood in the context of whole body health:
-
Hormone imbalances are found in a number of psychiatric conditions, such as abnormal levels of salivary cortisol, a hormone that helps the body respond to stress.
-
The immune system can trigger inflammation, which can appear in the bloodwork of patients with psychiatric and brain-based conditions.
-
The gastrointestinal (GI) system can contribute to symptoms of psychiatric illnesses during periods of imbalance and inflammation.
There Is Hope

With this functional medicine psychiatry approach, I have seen patients heal and improve in ways that I could not have imagined earlier in my career. Every day, patients in our clinic report that they are finally starting to feel better after suffering for years. They find a reason to be hopeful again.
If you are in California and would like to learn more about how our functional medicine approach could help you or a family member, please visit our website.
For those outside of our area of service who are interested in finding a doctor near you, you can visit the website for Integrative Medicine for Mental Health.
REFERENCES







