Patients with trauma or PTSD often wonder why they can’t move on from past events, even if they happened years ago. Through talk therapy, they may come to understand that they are no longer in danger, yet may continue to experience heightened anxiety, panic, flashbacks and nightmares.
This is because trauma affects more than just our thoughts. Trauma changes the brain and body in ways that talking and reasoning may not be able to reverse. Healing from trauma requires healing the brain and body’s biology, not just our thoughts.
Neurofeedback is one of the new promising, evidence-based therapies that can help address the deeper, underlying biological changes that result from trauma and PTSD. In this article, we address questions including:
- How does trauma affect the brain and body?
- What is neurofeedback treatment?
- Does neurofeedback help with trauma?
- What types of neurofeedback are helpful for trauma or PTSD?
Trauma Therapy: Talking might not be enough.
Talk therapy for trauma can be helpful in many ways, including:
- Validating emotions and helping patients realize that they are not to blame for what happened
- Looking at the traumatic event through a new lens
- Providing a sense of community, care, and support
However, trauma is stored in deeper parts of the brain and nervous system as whole-body experiences, not just linear narratives. This means that patients don’t just remember what happened as a coherent story – they also remember how they felt and how their bodies reacted. They remember how scared they were, as well as their racing heart and difficulty breathing.
Talk therapy often cannot address these emotional and physical memories of trauma that have become ingrained in the body’s biology.
Additionally, one study found that about 40% of patients in the community with PTSD drop out from CBT (cognitive behavioral therapy), the most recommended type of talk therapy for trauma. Patients need a more comprehensive type of treatment with better outcomes.
How does trauma affect the brain and body?
How does trauma change the Brain?
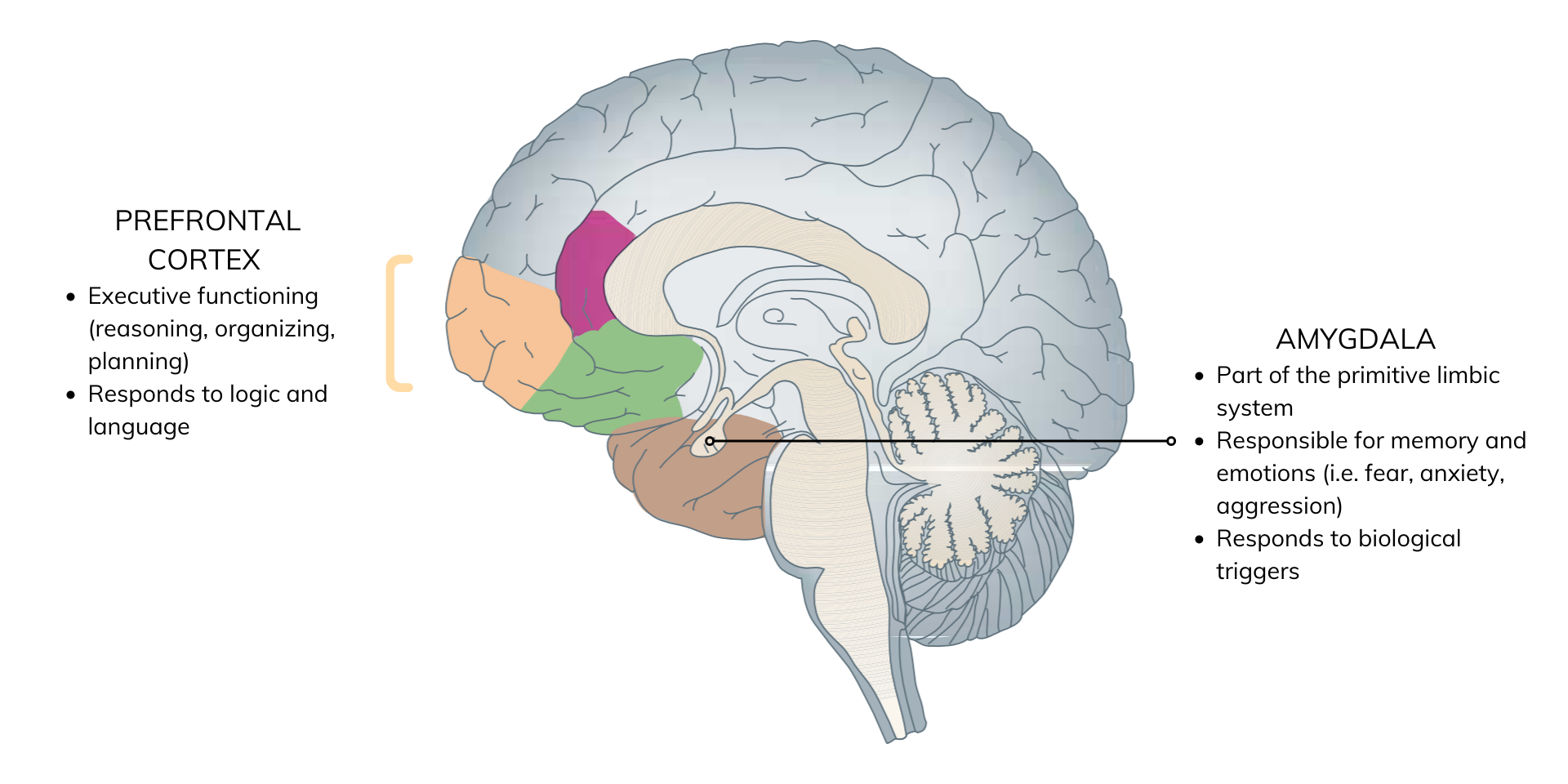
Trauma takes away a person’s sense of safety and stability at a deep, core level and activates the amygdala. The amygdala is part of the limbic system, a deeper, more primitive part of the brain that primarily responds to basic signals about fear and safety. Here, memory is stored as a lived experience with feelings and physical sensations that may not be connected in a logical story.
Talk therapy works at the prefrontal cortex where we plan, learn, and organize, but it does not communicate as well with the limbic system. In other words, talk therapy can appeal to our sense of reasoning and language, but it doesn’t speak to the deeper parts of the brain that experience and store the memories of trauma.
“the body keeps score”: Trauma & the body
During a traumatic event, the amygdala alerts the hypothalamus, a part of the brain that coordinates the body’s stress response by producing hormones like cortisol. In addition, the autonomic nervous system – which controls our involuntary body functions – goes into fight-or-flight mode. This means having a faster heart rate, breathing more shallowly, sweating, and not being able to think clearly.
In this way, trauma can change the body’s biology. Even after the trigger is gone, the amygdala can hold onto the physical memory of trauma, and our bodies can get stuck in this fight-or-flight mode, leaving us with higher levels of cortisol and symptoms of hyperarousal.
New treatments for calming the Brain & body after trauma
While we can ask someone to calm down and think more rationally, that may not change their whole-body response to trauma. We need trauma treatments that can heal the brain and body’s biology.
>
“Traditionally we’ve tried to heal PTSD through talking and making meaning of the event, but treatment methods that help calm arousal systems in the deeper regions of the brain have been helpful in calming PTSD more than those that try to do so through talking and reasoning.”
— Dr. Bessel van der Kolk, author of “The Body Keeps Score”
One of the promising treatments for calming the body and speaking to the deeper parts of the brain is neurofeedback.
What is neurofeedback therapy?
Neurofeedback is a non-invasive, evidence-based treatment that can encourage healthier brain function through brainwave training.
Our brain cells communicate through electrical impulses, also known as brainwaves. Normal brainwave patterns can be disrupted by trauma, resulting in patients getting stuck in unhealthy patterns of biological activity and behavior. Neurofeedback can help the brain become more flexible and develop healthier patterns and responses, a process known as neuroplasticity.
How does neurofeedback work?
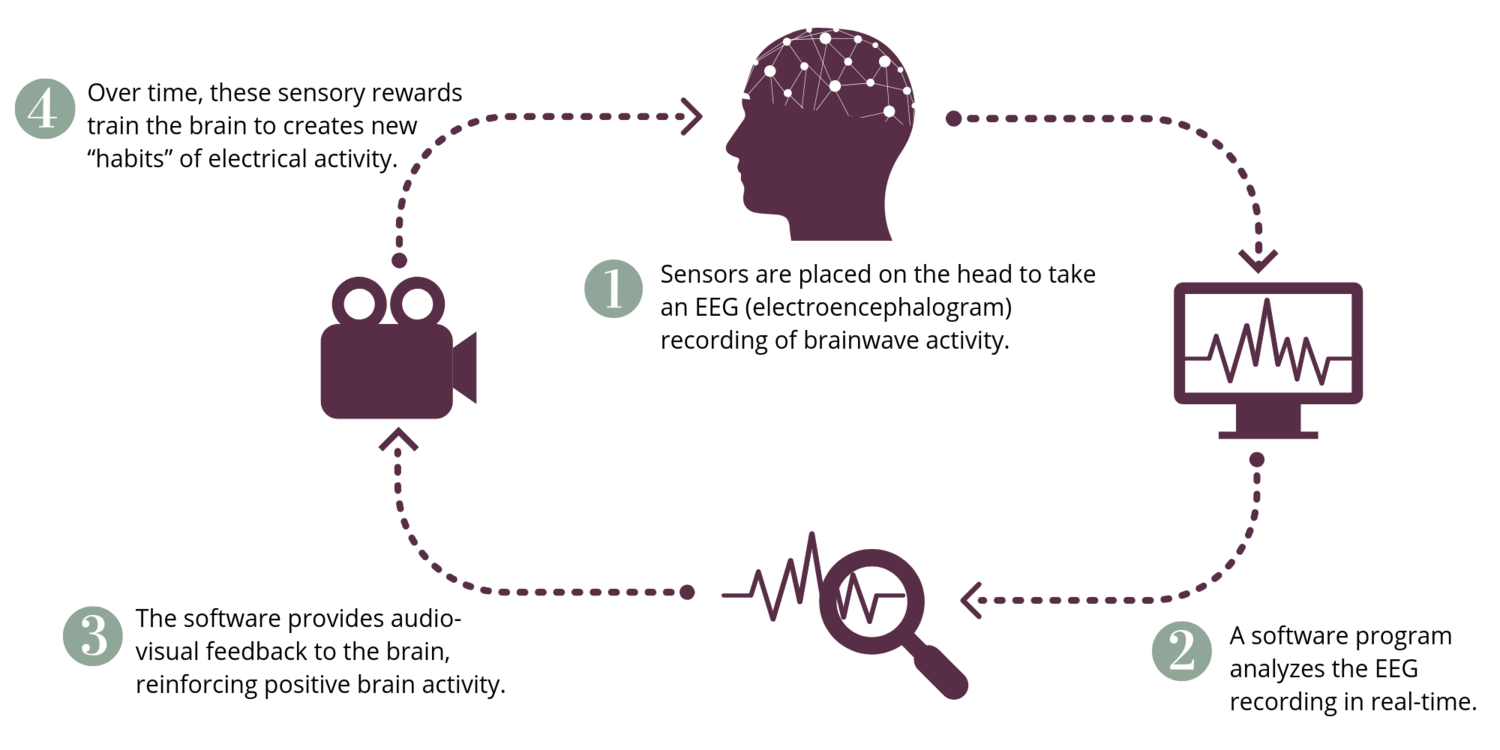
When a patient’s brainwave activity moves into a healthier state, the brain is rewarded with pleasant video and audio. Our brains, just like animals, are constantly seeking rewards. During a single neurofeedback session, the brain is given multiple opportunities to self-correct and be rewarded.
Since neurofeedback doesn’t require patients to talk about past events, they can relax and let their brains do the work for them. However, it is important that patients have a licensed mental health provider to speak to if associations, feelings, or memories come up during or after the session.
Does neurofeedback therapy help with trauma? What’s the evidence?
The goal of trauma-focused neurofeedback is to help shift people from a hyper-aroused state to a calmer one so that they can experience a sense of safety and react more appropriately to everyday events.
There have been many studies showing that neurofeedback can help with symptoms of PTSD. Some have even shown that neurofeedback can change brain function of PTSD patients on imaging or fMRI.
Furthermore, the level of symptom improvement in most of these studies has been significant. In fact, the effect size with neurofeedback in many studies has been greater than any medication used for PTSD.
One limitation of current research is that the number of people involved in each study has been relatively small. This is unsurprising, as it is challenging to deliver neurofeedback to large groups of people given the time, space, trained staff, and specialty equipment needed for treatment. Future studies that are larger and better-designed will provide us with more insight into the benefits of neurofeedback.
What types of neurofeedback therapy are helpful for trauma or PTSD?
Neurofeedback is an umbrella term that refers to many different types of brainwave training. There are two types of neurofeedback that seem to be especially helpful for trauma patients based on clinical research:
1. ILF (infra-low frequency) Training for Trauma
What is it? This form of neurofeedback trains the slowest brainwaves that are involved in regulating the brain’s stress response. If this response isn’t properly regulated, the brain can easily be triggered by even the smallest of events.
What do patients experience during a session? The goal of ILF treatment is to help the brain move to a less aroused and calmer state. Patients often report feeling physically and emotionally calmer after these sessions. Research and clinical observations find that patients often experience a change in their heart rate, muscle tension, and skin temperature as they move out of fight-or-flight mode into a calmer, more relaxed state.
2. Alpha-theta Training for Trauma
What is it? This type of training encourages alpha and theta brainwave activity, both of which are associated with introspection and relaxation.
What do patients experience during a session? When patients have an increase in both of these brainwaves, they can enter a deep state between wakefulness and sleep. In this state, people are more open to processing things in a new and healthier way.
After these sessions, patients may find that when they think about past events or traumas, they have more insight into their emotions without feeling disabled, distressed, or overwhelmed.
Integrating ILF and Alpha-Theta Treatment
Patients in our clinic typically do ILF treatment before alpha-theta training, allowing them to experience a sense of calm and safety before processing trauma. Even though patients are not required to think or talk about their trauma, some patients may find that memories or associations come up during or after a session. For this reason, it is important that a mental health practitioner is present when patients are doing neurofeedback training.
New Avenues for Healing from Trauma
Patients who haven’t recovered with talk therapy shouldn’t feel alone. Trauma is a devastating event that has long-term effects on the brain and body. There are deep biological reasons for why patients may need additional treatments.
During the last 15 years, I have researched and evaluated a number of different trauma treatments. In my experience, neurofeedback stands out as one of the most helpful treatments for patients with trauma. Years of research and clinical experience of doctors like myself support the potential of neurofeedback to help many more.
If you are interested in reviewing the research on neurofeedback, please visit our website. If you would like to learn more about ILF and alpha-theta training, you can visit the EEG Institute.
References
1. “The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma” Bessel van der Kolk (2014)
2. “Restoring the Brain: Neurofeedback as an Integrative Approach to Health” Hanno W. Kirk (2015)
3. “A Randomized Controlled Study of Neurofeedback for Chronic PTSD” PLOS (2016)
4. “Electroencephalography-based neurofeedback as treatment for post-traumatic stress disorder: A systematic review and meta-analysis” Cambridge University Press (2020)
5. “Current Status of Neurofeedback for Post-traumatic Stress Disorder: A Systematic Review and the Possibility of Decoded Neurofeedback” Frontiers in Human Neuroscience (2019)
6. “A Pilot Study of Neurofeedback for Chronic PTSD” Applied Psychophysiology and Biofeedback (2016)
7. “Post Traumatic Stress Disorder—The Neurofeedback Remedy” Biofeedback (2009)
The information and any products mentioned in this article are not intended to diagnose, treat, cure, or prevent any disease. The information provided is for educational purposes only and not intended to replace the relationships with your physician(s). Before initiating any conventional or integrative treatments, please first consult with a licensed medical provider. Please review references cited at the end of article for scientific support of any claims made.
Suruchi Chandra, MD
By
April 17, 2021
|







