In reality, depression is a much more complex condition that stems from many different causes.
In this article, we’ll share a new framework for understanding depression as a whole-body condition, as well as some of the recent research around the biological causes of depression. We discuss questions including:
As a psychiatrist using the integrative medicine approach for over 15 years, I have seen many patients who did not improve with talk therapy and antidepressants finally get the answers and treatment that they desperately need through this new framework of depression.
Is depression caused by a chemical imbalance?
If you think the answer is yes, you’re not alone. According to one survey, over 80% of people think that depression is due to a chemical imbalance in the brain.
While it is true that low levels of neurotransmitters like serotonin or norepinephrine can play a role in depression for some people, this is only one piece of a much larger puzzle. In fact, the chemical imbalance theory has not been proven as the main cause of depression in over 50 years of research. Multiple studies have found that decreasing the levels of tryptophan (the building block for serotonin) has not consistently led to depression or other mood disorders.
While simple explanations like the chemical imbalance theory may be easy to understand, they don’t capture the whole picture of the brain’s activity and relationship to the rest of the body. New research shows how the brain is more like a complex computational system with intricate networks and connections.
Antidepressant medications like SSRIs (ex. Zoloft, Lexapro, Prozac) target chemical imbalances in the brain, such as low serotonin or norepinephrine activity or other dysregulated levels of neurotransmitters. While this has been helpful for some people, one study found that only 46% of patients get fully well when receiving a combination of antidepressants and talk therapy.
This isn’t surprising as we now know that depression is caused by more than a chemical imbalance in the brain. Even those who see some improvement with SSRIs and other antidepressants may continue to have symptoms such as loss of interest, difficulty sleeping, or emotional numbness. People may also experience side-effects that are uncomfortable or undesirable, which may result in them stopping treatment.
In order to help those who haven’t improved with antidepressants, we have to look beyond the chemical imbalance theory to other causes of depression.
Is depression genetic?
Some people feel like they’re destined to live with their condition if they have a family history of depression or other mood disorders. Sometimes they’re convinced that it’s “in their genes.”
However, research shows that genes don’t determine your destiny with depression. In addition to genetics, factors like the environment, life events and stressors, and our everyday health choices all play an important role in the development of depression.
In one study from Harvard, researchers found that a moderate amount of regular exercise could offset the genetic risk factors for major depressive disorder. It’s likely that other lifestyle choices that we make, such as our eating habits and sleep routine, have a similar effect.
IS THERE A “DEPRESSION GENE”?
While it’s true that your chances of developing depression increase if another family member has it, there isn’t one single gene that determines depression. On the other hand, inherited disorders like cystic fibrosis or Huntington’s disease have a clearly defined gene mutation or genetic cause.
So far, the search for a single gene that can cause depression has been elusive. Instead, there seem to be many genes that contribute to depression, each of which has only a small effect. This points to depression being a complex condition with many different causes.
What are the causes of depression?
THE ROLE OF STRESS IN DEPRESSION
There is clear evidence showing that emotional and social stress can lead to clinical depression. While it may seem intuitive how stress can contribute to symptoms of depression, stress doesn’t just make us feel overwhelmed and frazzled: it changes our biology.
Stress can trigger the release of hormones and other chemicals that affect many systems in the body. For example, stress can lead to inflammation, changes in blood sugar and the gut microbiome, and more.
When our bodies are not healthy, this response to stress can become exaggerated, leading to chronic or higher levels of inflammation and other changes. This can set the stage for depression.
THE ROLE OF BIOLOGY IN DEPRESSION: A WHOLE-BODY CONDITION
Research has now proven that when it comes to mental health, it truly isn’t all in your head. For depression, mood disorders, and other mental illnesses, we have to consider the health of the body as a whole.
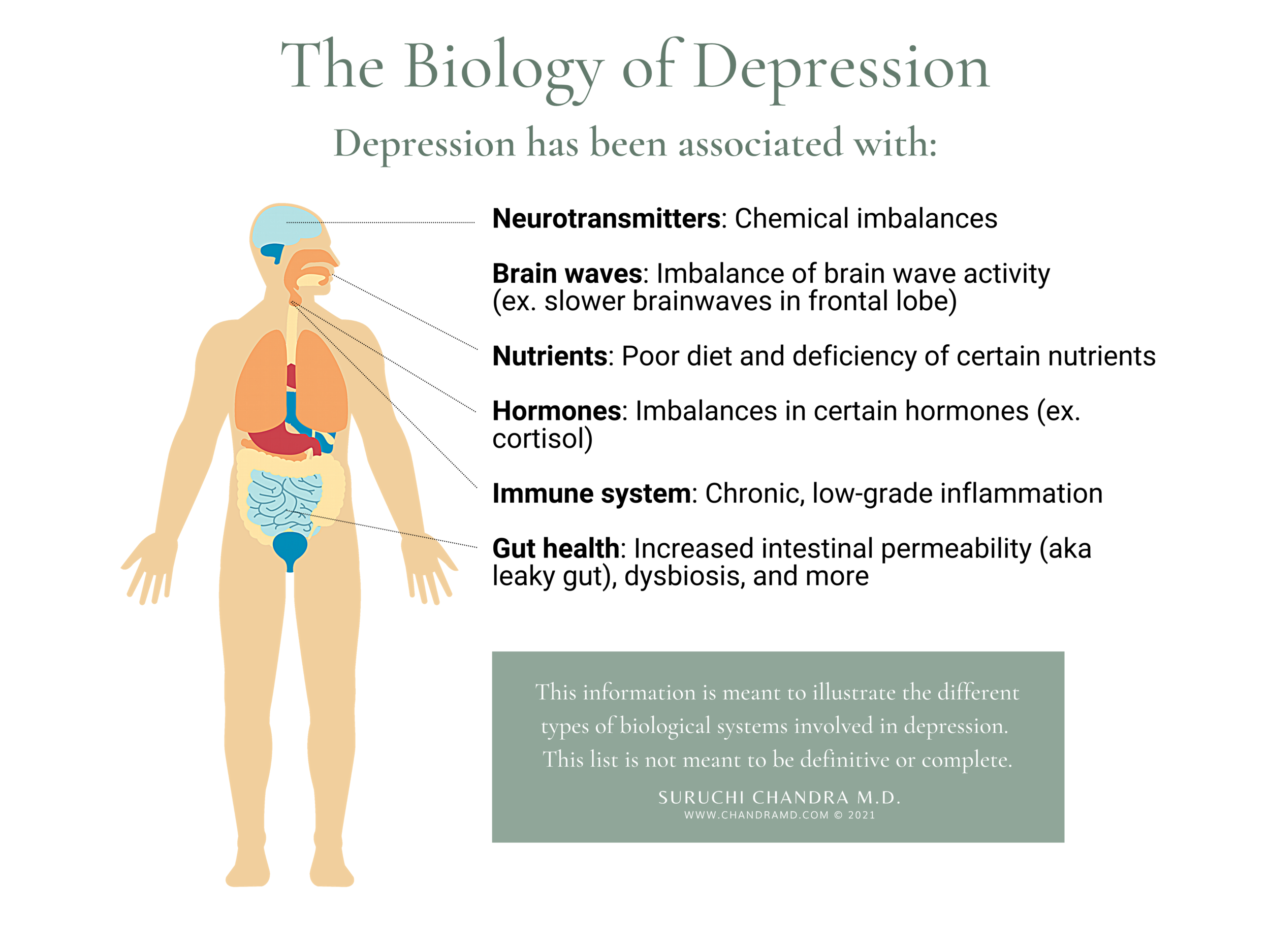
In this section, we review the body systems that are currently thought to be most involved in stress and depression. Because this is an emerging field, this information is meant to illustrate the different types of biological issues we should be thinking about and is not meant to be definitive or complete.
BRAIN WAVES
In addition to chemicals, our brain cells also communicate through electrical impulses called brain waves. These waves vary in speed and are associated with different activities, from problem-solving to sleep. Too many slow brain waves in the front of the brain have been associated with major depressive disorder, lack of motivation, and feeling sad. A targeted way to address this type of imbalance is through neurofeedback and neuromodulation, which are aimed at encouraging healthier brainwave patterns.
IMMUNE SYSTEM & INFLAMMATION
Inflammation is the body’s response to a perceived threat, such as a cut or infection. When it becomes widespread or chronic, it can wreak havoc in the body and brain. In fact, studies show that chronic, low-grade inflammation is associated with increased risk for depression and other mental illnesses. Possible sources of inflammation include poor diet, stress, changes in the gut microbiome, and certain medical illnesses.
GUT-BRAIN AXIS
The gut is sometimes called the second brain because it has a rich network of nerve cells and neurotransmitters. Not surprisingly, disruptions in gut health can impact how we feel and think. About 70% of our immune system is housed in the gut, so when immune cells sense a breach in the integrity of the gut lining, they sound the alarm by spreading inflammation throughout the body. Learn more about the connection between gut health and depression here.
HORMONES
Hormones (ex. cortisol, estrogen, thyroid hormones) are chemicals that are produced by the glands and travel through the blood to other parts of the body, including the brain. These chemicals are critical for brain function and health, and imbalances in certain hormones can lead to low mood and depression. These imbalances can happen for many reasons, including stress, poor diet, aging, and inflammation.
NUTRIENTS: THE LINK BETWEEN FOOD & MOOD
Food is more than energy for the brain. It also provides the building blocks for neurotransmitters and brain cells, as well as antioxidants to protect against inflammation. Not surprisingly, there is a growing body of evidence supporting a link between what we eat and our mental health. A review of the medical literature found that seafood, leafy greens, and cruciferous vegetables were the most helpful in preventing and recovering from depression.
A New Framework for Understanding the Causes of Depression

Chemical imbalances, genetics, and stress are all risk factors that play a supporting role in a much larger picture of depression. To fully understand the biological causes of depression, we have to use a bigger lens to look beyond the brain at the different body systems involved and their complex interactions.
While this may seem overwhelming at first, it gives us a reason to be hopeful. Because there are so many possible causes of depression, this means that there are just as many opportunities for healing beyond talk therapy and medications. Partnering with a doctor who considers comprehensive testing and treatment and uses a functional medicine approach to mental health may help you better understand these possibilities and find new avenues for healing.
References