Neurofeedback, also known as EEG biofeedback, has been gaining more attention as a non-invasive, medication-free approach for treating brain-based conditions, including ADHD, anxiety disorders, and even autism. Still, many people question, “Does neurofeedback actually work?”
When I first encountered neurofeedback 15 years ago, I was also skeptical. If it was effective, why hadn’t I heard about it during my psychiatry training at Harvard? Over the next few years, I witnessed how it helped some of my patients with anxiety, sleep, and focus issues, motivating me to do more investigation and training. Now, neurofeedback is integral to my clinic’s work.
In this article, I’ll address the most common questions that my patients ask me about this type of treatment:
- What is neurofeedback?
- How does it work?
- What can it treat? What is it used for?
- What are the different types of neurofeedback?
- Does neurofeedback work?
- Is it safe? Are there side-effects?
- What should I expect from treatment?
- Is treatment covered by insurance?
- How do I find a neurofeedback center near me?
What is neurofeedback therapy?
Neurofeedback is a non-invasive treatment that encourages the brain to develop healthier patterns of activity. The goal of treatment is not only to change how you think and feel, but also to change your brain on a biological level for better functioning.
Recent research has shown that when given the proper support, the brain has the ability to change and adapt, a property known as neuroplasticity. Neurofeedback can encourage and speed up this process of neuroplasticity.
Words alone are often not enough. Simply telling someone to calm down or focus doesn’t solve the underlying issues of conditions like anxiety or ADHD. On the other hand, neurofeedback allows us to speak to the brain with its own language: brain waves.
What is a brain wave?
Our brain cells communicate through electrical impulses known as brain waves. Each brain wave has two properties:
- Frequency, which is how fast the wave travels.
- Amplitude, which is how tall the wave gets when it goes up and down.
In general, faster brain waves are associated with focus, thinking, and awareness, while slower brain waves are associated with relaxation, meditation, and deep sleep.
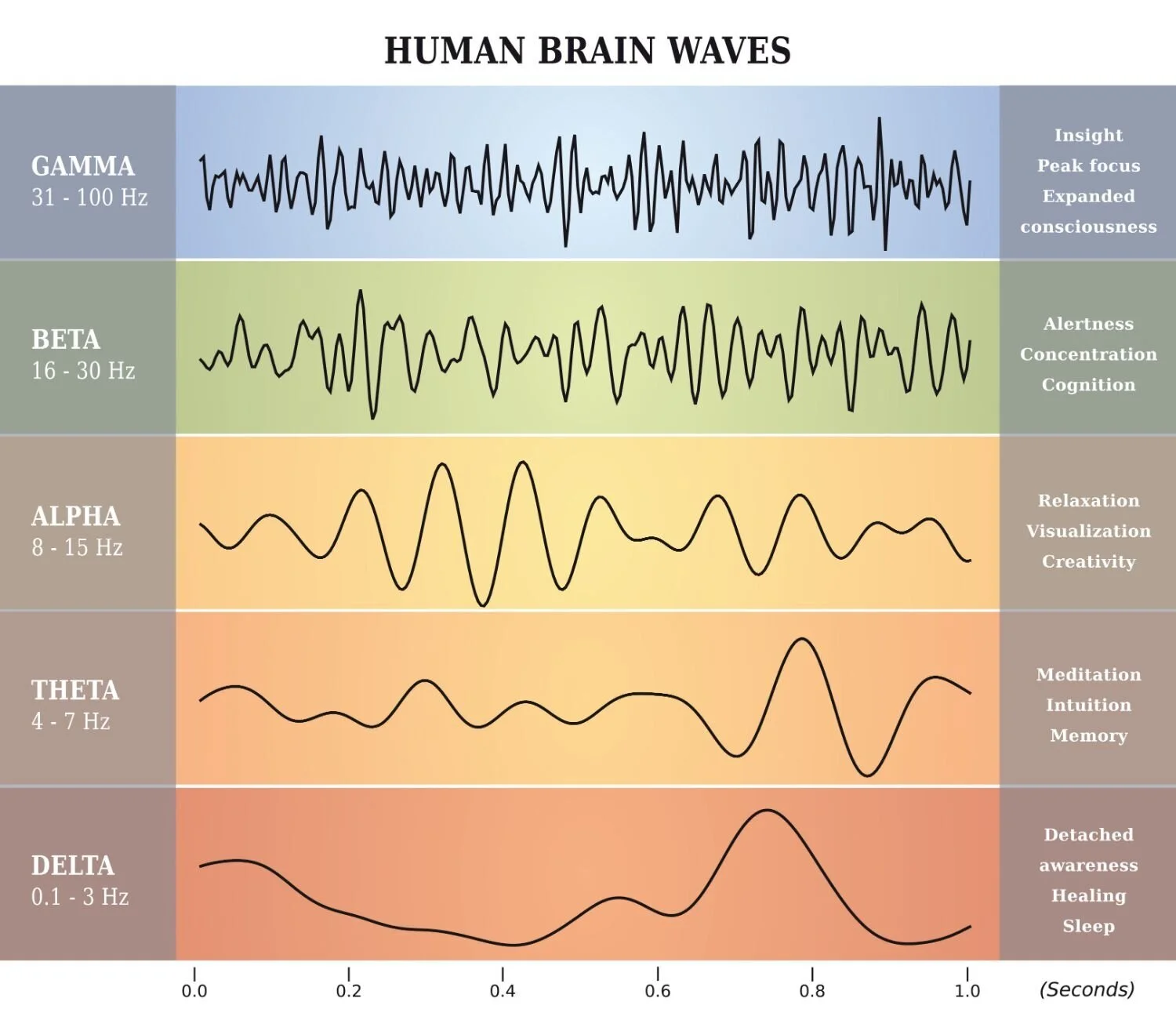
In mental health disorders, brain wave patterns can become disrupted, leading to unhealthy biological activity and behavior. For example, people with anxiety disorders often have too much fast brain wave activity, which leaves them feeling on edge, hyper-aroused, and panicky. On the other hand, those with ADHD can have an excess of slower brain wave activity, resulting in symptoms like brain fog, daydreaming, and trouble focusing.
The goal of neurofeedback therapy is to help modulate these dysregulated brain wave patterns.
How does neurofeedback work?
A typical neurofeedback session follows these basic steps:
- Set goals for treatment. Goals are based on a patient’s condition and the type of neurofeedback system. For example, the goal of anxiety treatment may be to regulate fast brain wave activity so that a patient feels calmer and more relaxed after a session.
- Measure brain wave activity. A clinician starts by placing electrodes on a patient’s scalp to obtain a real-time measurement of their brain waves (i.e. electroencephalography, or EEG). After set-up, the patient may watch a movie, play a video game, or listen to music as neurofeedback training begins.
- Train the brain with positive feedback. When the EEG detects that a patient’s brain wave activity has met the goals of treatment, the brain is rewarded with positive feedback. For a patient with anxiety, they may be rewarded with a larger movie screen, higher score on the video game, or pleasant audio feedback when their brain makes more of the slower alpha waves and less of the faster beta waves.
- Repeat training. The EEG continues to monitor the patient’s brain waves and give positive feedback when goals of treatment are met. This training loop gives the brain thousands of opportunities to self-correct and be rewarded in one session.
Training the brain with positive feedback is based on the principles of learning theory, or operant conditioning, and is similar to how we train a dog to sit by rewarding it with a treat. Our brains, like animals, are constantly seeking rewards.
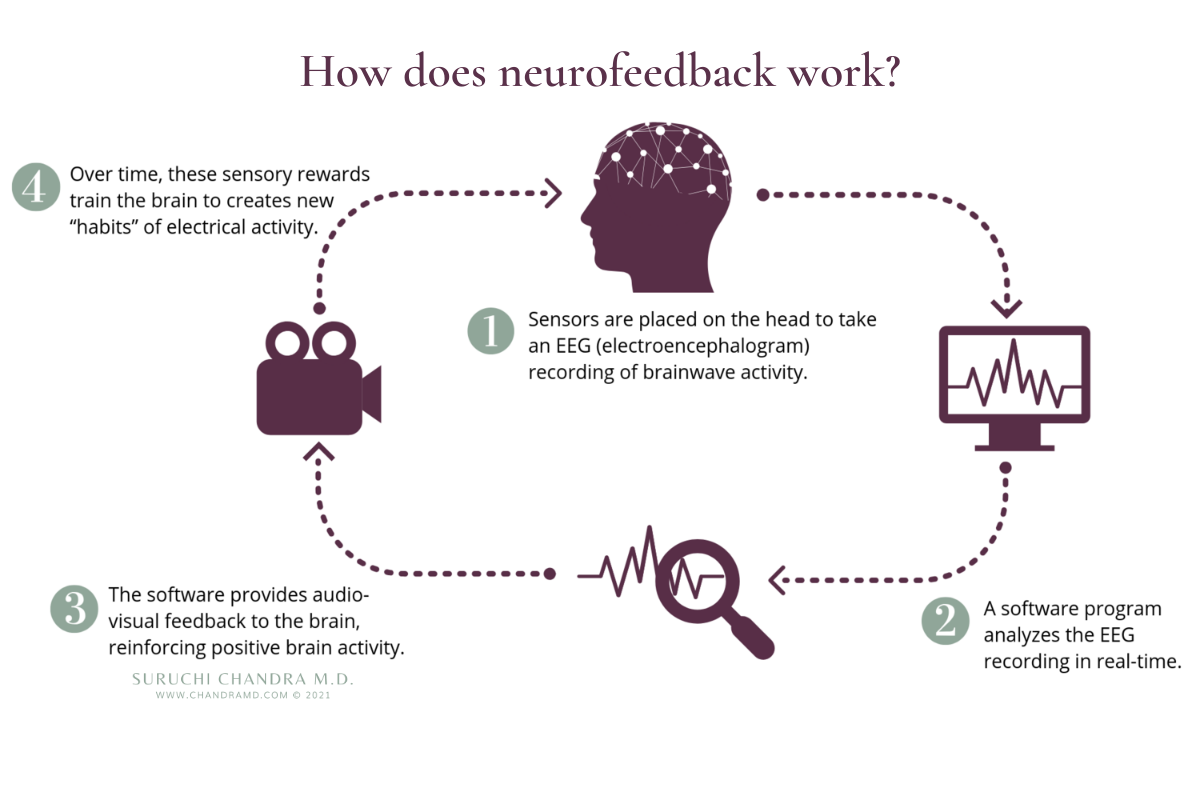
Notably, neurofeedback does not involve any electrical current or stimulation of the brain like some other brain-based therapies (ex. TMS, LENS, or tDCS).
In a nutshell: Our brains use brain waves to communicate and function properly. These brain waves may become dysregulated, which can lead to psychiatric or neurological symptoms. Neurofeedback is a non-invasive treatment that addresses imbalances in brain wave activity to help patients achieve deeper healing and better functioning.
What can neurofeedback treat? What is it used for?
Because brain waves are involved in all brain activity and functions, this treatment can be used for a wide range of brain-based conditions:
MENTAL HEALTH ISSUES & PSYCHIATRIC DISORDERS
Includes those with mood & anxiety issues, OCD, panic, or PTSD
Neurofeedback can help patients feel calmer, happier, and safer. For example, treatment for anxiety disorders may involve reducing excess fast beta waves (associated with anxiety) and increasing alpha waves (associated with calmness).

DEVELOPMENTAL DELAYS & BEHAVIOR DISORDERS
Includes those with ASD, attention deficiency (ADHD), or PANS/PANDAS
For many developmental disorders, the brain does not develop the proper networks for communication. In children with autism, neurofeedback can significantly change the brain networks as detected on fMRI imaging and improve behavior.

NEUROLOGICAL ISSUES & BRAIN INJURIES
Includes those who have had TBI, stroke, tinnitus, or Parkinson’s
For these conditions, neurofeedback offers hope for new ways of healing, especially when combined with an integrative approach to medicine.

PEAK PERFORMANCE
Includes athletes, executives, and students who want to excel
Neurofeedback is like exercise for the brain and can help even those who don’t have psychiatric or neurological disorders achieve optimal functioning.
What are the different types of neurofeedback?
Neurofeedback is an umbrella term that refers to several different types of EEG biofeedback systems. The various types differ on the type of brain waves being trained, goals of therapy, and number of targeted sites in the brain.
The most common types of neurofeedback are:
- Amplitude training: This is the original and still most popular approach in the field. It focuses on increasing or decreasing the size of certain brain waves.
- Slow cortical training (ILF, ISF, and SCP): This approach trains the slowest brain waves, which can help with emotional regulation and brain stabilization.
- Z-score training: The goal of this approach is to encourage a patient’s brain wave activity to move towards the norm or average of healthy people.
At this time, we can’t say conclusively what the best type of neurofeedback training is because there have been few comparative studies between systems.
The takeaway: The wide variety of systems is both an opportunity and a challenge for the field. It allows for individualized care and opportunities for novel ways of healing. However, finding the best system for your needs can be a challenge, as there are few comparative studies. Like other forms of exercise and physical training, combining different types of neurofeedback training may be optimal for brain health.
Does neurofeedback work?
Asking “Does neurofeedback work?” is similar to asking if all medications work. The answer is more complicated than a simple yes or no. The results depend on many factors, like whether the treatment is the right fit for a patient’s condition or ability of the treatment to change a patient’s brain biology. For example, some people may not see benefits from neurofeedback because they are not using the right system for their needs.
Most of the clinicians in this field, including myself, continue to use neurofeedback because we have seen it work and improve patients’ conditions when applied properly.
There are numerous studies that support its clinical use. In some studies, patients not only felt better after treatment, but imaging technology (i.e. fMRI) showed that the treatment actually changed patients’ brain function and structure.
THE FUTURE OF NEUROFEEDBACK RESEARCH
Some researchers have cautioned that the current evidence is insufficient to make any conclusive claims. They point out that many of the studies are small in scale, and some are not randomized controlled trials or have other design flaws.
However, academic centers like Stanford University consider the evidence behind neurofeedback promising enough to start their own clinical trials. As the field advances, we will hopefully have better-designed studies and better ways of understanding how neurofeedback changes the brain.
The takeaway: Neurofeedback is based on sound scientific principles and numerous clinical studies. There is enough evidence that it should be considered promising, especially in a field that has a great need for better treatment options. However, we still need more rigorous neurofeedback studies to conclusively determine not only if it works, but exactly how it works and the best systems.
Is neurofeedback safe? Are there any side-effects?
Because neurofeedback is a non-invasive treatment as well as a form of exercise for the brain, it is generally considered safe without significant side effects.
When side-effects do occur, they are typically short-lived and usually resolve within 24 – 48 hours. The most common side-effects include sleepiness, lack of focus, mild headaches, and anxiety. In one review for patients with ADD / ADHD, this side-effect only occurred in about 1-3% of patients.
It’s important that patients report side-effects to their clinician so they can modify the treatment. As long as the proper adjustments are made and you are working with a qualified and licensed mental health practitioner, there shouldn’t be any long-term symptoms or consequences.
What should I expect from neurofeedback training?

Changes to the brain typically happen slowly and over time. For that reason, it can take many sessions to achieve long-term changes in symptoms and brain functioning. Like all forms of exercise and therapy, it’s best to do neurofeedback training on a regular schedule, usually 2-3 times a week.
To determine response to treatment: Most systems may take between 10 – 20 sessions before a patient can tell if treatment is helping. Slow-wave training systems (i.e. ILF, ISF, and SCP) may take 1- 5 sessions.
To consolidate long-term benefits: 30-40 sessions are typically recommended for all systems. For more complicated conditions such as autism, other developmental delays, and brain injury, more sessions may be needed.
WILL THE RESULTS OF NEUROFEEDBACK LAST?
Because neurofeedback encourages neuroplasticity, it has the potential to result in longer-lasting adjustments in brain functioning. Many clinicians see patients who have achieved long-term benefits over many months or years, however, the research has not been conclusive.
Is neurofeedback covered by insurance?
Neurofeedback has valid reimbursable insurance CPT codes. However, some insurance companies do not cover this type of treatment. Because reimbursement varies, we recommend that you contact your insurance company to find out what your particular plan offers.
Typically, companies will cover neurofeedback sessions if a licensed medical professional or therapist is present for talk therapy or psychotherapy.
How do I find a neurofeedback center near me?
Finding the right neurofeedback clinic for your needs can feel overwhelming and confusing. Try to find a center with:
- Clinicians who have certification and proper training. Biofeedback Certification International Alliance (BCIA) and the Othmer method have their own certifications.
- Clinicians who have experience in the field of mental or brain health (ex. psychologist, psychiatrist, social worker).
- Neurofeedback systems that have FDA clearance.
- Expertise in your condition or challenges.
BCIA has a database of providers with a wide variety of neurofeedback services. EEG Info offers clinical care and education for ILF neurofeedback and provides a database with practitioners trained in this method.
Why choose neurofeedback?

Neurofeedback can be a powerful tool for healing in a field that desperately needs better treatment options. By directly targeting specific sites in the brain and changing the brain’s biology for better functioning, it has the potential for long-term benefits. In my clinic, neurofeedback continues to surprise me and my patients with its ability to heal the brain in new ways.
While the field still needs more research to help us understand the exact mechanisms behind neuroplasticity and EEG biofeedback, this is a promising treatment option when administered properly. As the field progresses, I hope that neurofeedback is considered as a serious treatment option by both clinicians and patients.
References
1. “Direct modulation of aberrant brain network connectivity through real-time NeuroFeedback” – National Institute of Mental Health (2017), DOI: 10.7554/eLife.28974.001
2. “Transient Adverse Side Effects During Neurofeedback Training: A Randomized, Sham-Controlled, Double Blind Study” – Applied Psychophysiology & Biofeedback (2015), DOI: 10.1007/s10484-015-9289-6
3. “Assessing the Effectiveness of Neurofeedback Training in the Context of Clinical and Social Neuroscience” – Brain Sciences (2017), DOI: 10.3390/brainsci7080095
4. “Neurofeedback: A Comprehensive Review on System Design, Methodology and Clinical Applications” – Basic and Clinical Neuroscience (2016), DOI: 10.15412/J.BCN.03070208
5. “The use of EEG Biofeedback/Neurofeedback in psychiatric rehabilitation” – Psychiatria Polska (2017), DOI: 10.12740/PP/68919
6. “EEG neurofeedback research: A fertile ground for psychiatry?” – L’Encéphale (2019), DOI: 10.1016/j.encep.2019.02.001
The information and any products mentioned in this article are not intended to diagnose, treat, cure, or prevent any disease. The information provided is for educational purposes only and not intended to replace the relationships with your physician(s). Before initiating any conventional or integrative treatments, please first consult with a licensed medical provider. Please review references cited at the end of article for scientific support of any claims made.
Suruchi Chandra, MD
By
August 24, 2021
|







