In psychiatry, we have limited our focus to the imbalances of neurotransmitters like serotonin in the brain. However, new research shows us that brain health is connected to whole body health, especially gut health. If we continue to overlook this relationship, we may leave many patients without the treatment that they need.
We need new approaches for understanding and treating depression and other mental health conditions.
According to one study, only 46% of patients have full resolution of depressive symptoms when receiving a combination of talk therapy and medication. This means that our current treatments, even when administered properly, may be missing the mark.
In the past ten years, there has been an explosion of literature showing the importance of gut health in psychiatric conditions. Specifically, there have been a number of studies that revealed a link between biomarkers for a leaky gut and occurrence of depression and suicidality. One study even found that the levels of biomarkers directly correlated with severity of suicidal symptoms.
One of the limitations of these studies is their small sample size, and larger studies in the future may give us more conclusive evidence about the role of gut health in psychiatry. In the meantime, however, the current evidence encourages us to consider the whole body in mental health conditions, an approach that may help us better understand treatment-resistant depression.
What is a “leaky gut”? Is it a real medical condition?
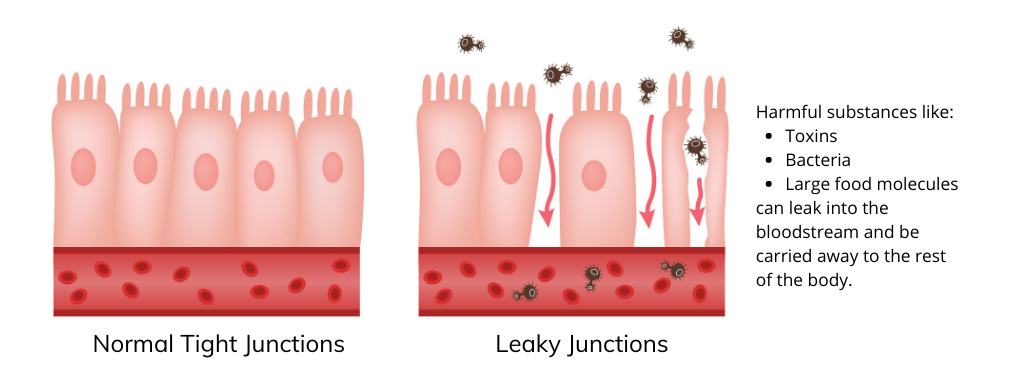
The gastrointestinal tract is the tube that connects our mouth to our colon. One of the functions of the GI tract is to form a barrier between our inner biological world and our external environment, allowing our bodies to absorb helpful nutrients while protecting us from harmful substances.
The cells lining the GI tract in our gut are joined together by proteins known as tight junctions. Under certain conditions, these tight junctions can become loose, causing the gut lining to have larger openings or holes that increase intestinal permeability, allowing harmful substances to “leak” into the bloodstream.
There is a strong growing body of evidence that intestinal permeability is both real and can contribute to a number of different neuropsychiatric disorders. Dr. Alessio Fasano at Harvard Medical School, one of the leading researchers in this field, has found probable links between intestinal permeability and a number of different diseases of the nervous system, including:
-
Multiple sclerosis
-
Autism spectrum disorders
-
Schizophrenia
-
Chronic fatigue
How is gut health related to depression & other mental health conditions?
When harmful substances leak out from the gut, they can cause a whole cascade of events to unfold. In addition to having direct toxic effects on the body and brain, these pathogens and toxins can also activate the immune system. About 70% of our immune system is housed in the gut, so when immune cells feel like there’s a breach in the integrity of the gut lining, they sound the alarm by spreading inflammation throughout the body. While a properly controlled immune system can be a helpful defense mechanism, an uncontrolled response may cause damage and lead to widespread inflammation in the body and brain.
Chronic inflammation caused by a leaky gut may result in psychiatric symptoms like anxiety and depression.
During periods of stress or inflammation, tryptophan, a building block for serotonin production, can be converted into kynurenic acid via the kynurenine pathway. If tryptophan continues down this path over a long period of time, chronic inflammation may result in the depletion of serotonin and creation of toxic substances in the brain. Through this pathway, the leaky gut can be connected to the common neurotransmitter imbalance that we see in anxiety and depression.
Could a leaky gut be the reason why I have treatment-resistant depression?
SSRI medications like Zoloft and Lexapro may help reduce psychiatric symptoms that are caused by low serotonin levels, which, in turn, may be a result of the widespread inflammation and activation of the kynurenine pathway due to a leaky gut. However, as they ultimately do not address the full cascade of events seen with a leaky gut, patients may feel like some of their symptoms have gotten better with SSRI medications but still don’t feel fully well. If you have depression that has not responded to conventional treatment, you may want to work with a provider who considers the gut-brain axis and looks beyond chemical imbalances in the brain, as the root cause of your health issues may be elsewhere.
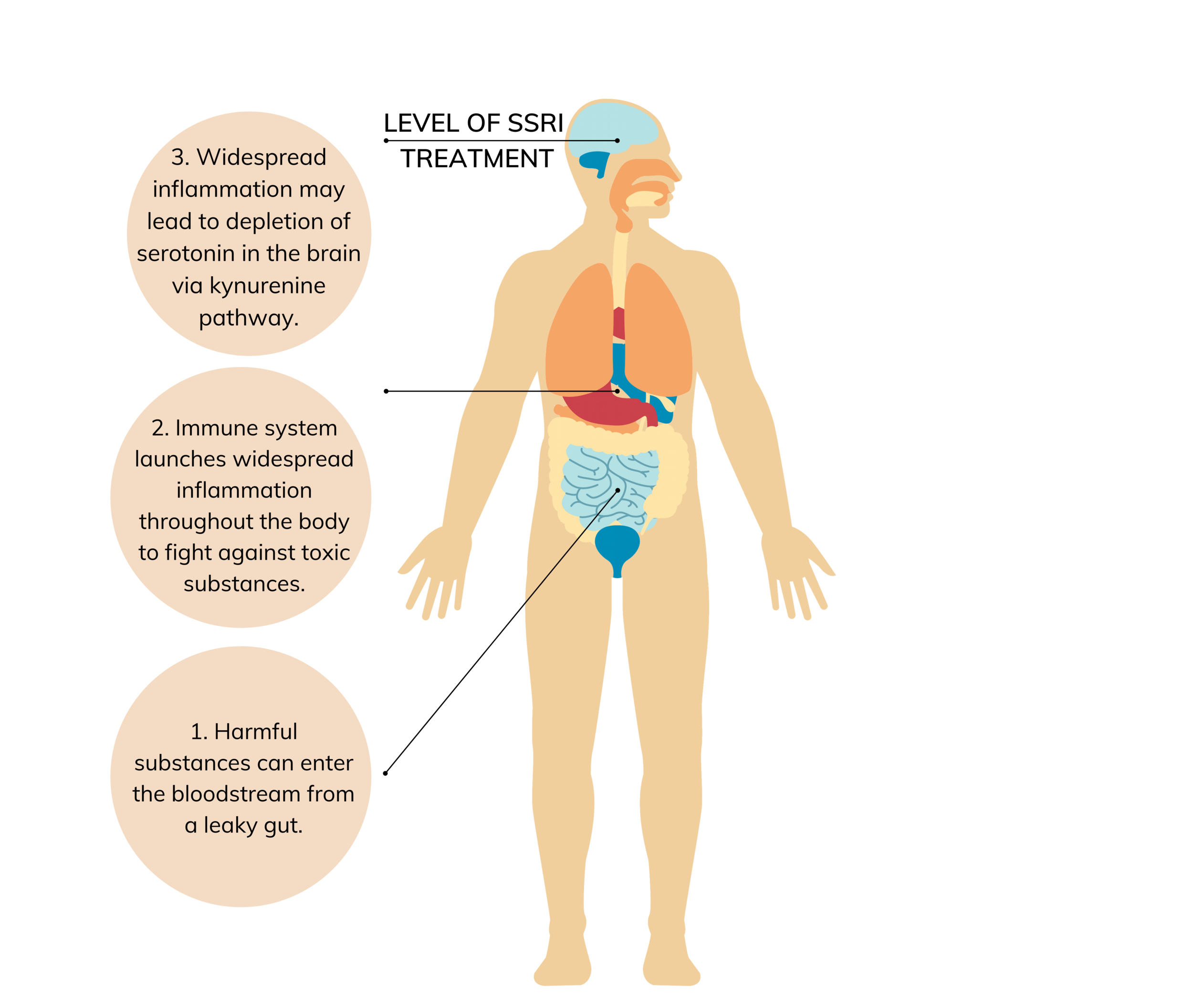
SSRI medications partially address psychiatric symptoms that may be caused by a leaky gut.
What contributes to a leaky gut?
To understand the leaky gut, it’s helpful to compare our external skin with our inner gut lining. Our skin was created with one main purpose: to protect and shield us from environmental threats. The epithelial cells that line our gut, however, have the complicated role of keeping out toxins while still allowing helpful nutrients and substances to enter our bodies. In order to achieve this goal, our gut lining is much more porous and delicate than our skin, and, as a result, is more prone to damage.
Many modern-day practices can cause damage to the epithelium, including:
-
Standard American diet high in processed foods, sugar, and gluten
-
Nutritional deficiencies, including zinc
-
Constant or frequent stress
-
Certain common medications, including antibiotics and proton pump inhibitors
-
Environmental toxins, including plastics (BPA) and pesticides
-
Certain conditions like obesity and diabetes
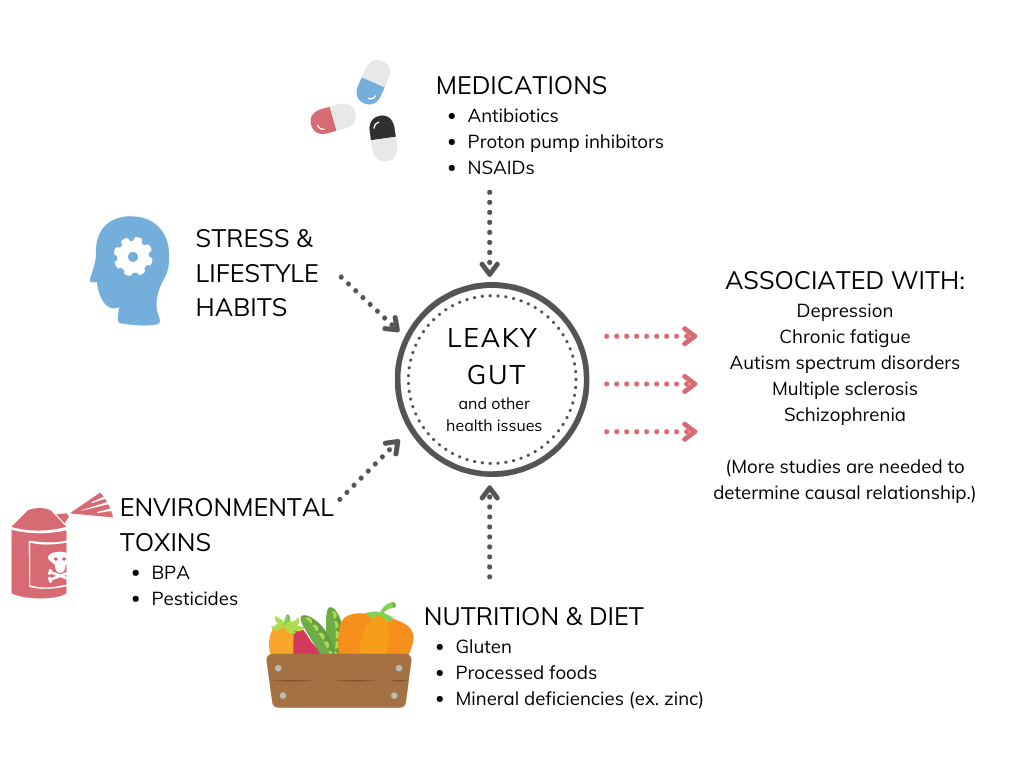
Various contributors to a leaky gut are part of the conveniences of modern every day life.
While a leaky gut is not the only contributor to psychiatric symptoms, it is one of several pathways that link these stressors to depression and other mental health disorders.
Does gluten really contribute to a leaky gut?
Researchers at Massachusetts General Hospital found that gliadin, a glycoprotein within gluten, increases intestinal permeability in all people. Yes, in everyone – not just those with gluten allergies or celiac disease. However, only some people experience symptoms or develop a disorder as a result of ingesting gluten. People who are more affected by gluten may have other stressors on their GI tract, such as poor diet or prolonged use of antibiotics, or genetic vulnerabilities that contribute to gut dysfunction.
Does a leaky gut always cause stomach symptoms such as abdominal pain or bloating?
Not everyone who has a leaky gut has stomach pain or even physical symptoms. Some patients only experience mood changes or other mental health issues, symptoms that are “downstream” from the problematic source of the leaky gut.
How do you treat a leaky gut?
1. Address and reverse the stressors that may have contributed in the first place. This could involve:
-
Eating whole, unprocessed foods
-
Practicing stress reduction techniques like yoga and meditation
-
Avoiding unnecessary medications
-
Avoiding environmental toxins when possible
2. Consider using protective and supportive herbs and supplements. Certain herbs and other supplements that may provide further healing in a leaky gut include:
-
Ayurvedic herbs like triphala
-
Prebiotic and probiotic supplements
Understanding the gut-brain axis can open up new pathways for healing, mentally and physically.
While there is evidence in research and my clinical experience that a leaky gut can contribute to depression, it is important to keep in mind that a leaky gut usually is not the only cause of mental health disorders. Addressing the leaky gut is foundational for many patients, but they may still need to work on trauma, other biological imbalances, or underlying infections to get to the root cause of their health issues.
As more studies reveal the extensive role that our gut plays in psychiatric disorders, we may develop a better understanding of treatment-resistant depression. Even current research shows us that we need better studies that look beyond serotonin imbalances in the brain and towards whole-body systems for deeper, more meaningful healing.
References







