It’s hard to watch someone that you care about struggle with an eating disorder. Even with therapy and treatment, they may continue to put themselves at risk for serious medical problems by starving themselves or exercising for hours on end.
Those who don’t improve with treatment are often seen as “unwilling” to get well or change their behaviors. However, it may not be their mindset that is treatment-resistant: it could be their biology.
While eating disorders are thought to be caused mainly by stressful life situations and social pressures, new evidence suggests that inflammation and infections can also play a role. Below, we discuss this evidence, as well as my clinical experience as a psychiatrist with using an integrative approach to address eating disorders like anorexia, bulimia, and binge eating disorder. We discuss questions including:
- What causes anorexia and other eating disorders?
- What is the link between eating disorders and infections?
- How can inflammation and infections cause an eating disorder?
- How are eating disorders and PANS & PANDAS related?
- How do you treat anorexia and other eating disorders?
What causes anorexia and other eating disorders?
There is no single cause for eating disorders. Each case is the result of a unique combination of factors that are biological, psychological, and social in nature. This is known as the biopsychosocial model in psychology.
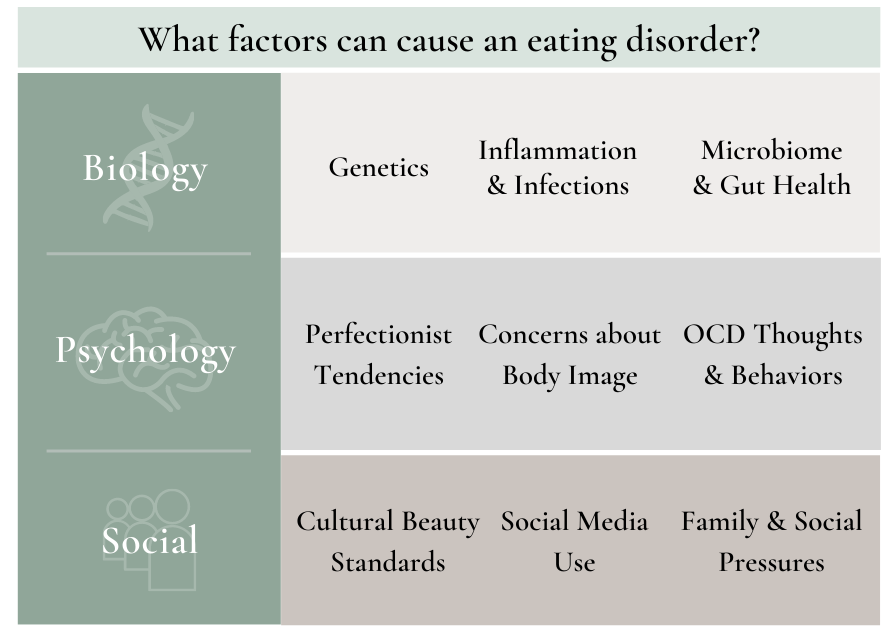
While people generally know about the psychological and social pressures that can lead to eating disorders, the biological factors are often overlooked, leaving many patients without a crucial part of their path to recovery.
Specifically, recognizing the role of inflammation and infections has become one of the most important pieces to helping patients in my practice who were previously thought to be treatment-resistant.
What is the research linking eating disorders and infections?
The relationship between eating disorders and infections has been studied in two main settings:
1. Reports of Eating Disorders Linked to Infections
Researchers have noticed that some people can develop eating disorders after getting an infection. Many of these reports were about children with PANS or PANDAS, a condition in which an infection can trigger OCD and tics, as well as sudden changes in eating attitudes and behaviors.
Some of these reports found that eating disorder behaviors decreased after antibiotic treatment for infectious triggers. Put simply, treating the infection also treated the eating disorder in these case reports.
Could this connection between infections and eating disorders be more common than we previously thought? A recent study at Massachusetts General Hospital (MGH) set out to answer this question.
2. Eating Disorders and Infections in the General Population
The MGH study evaluated over 500,000 teenage girls in Denmark and found that those who had been hospitalized for a serious infection or those who had completed more than 3 courses of antibiotics were 39% more likely to develop eating disorders.
While these results do not prove that infections cause eating disorders, they do encourage us to consider the role of infections and the immune system in eating disorders in general, and not just in children with PANS or PANDAS.
How can an infection cause an eating disorder?
At first glance, it may not be obvious how an infection could cause the changes in thinking and behaviors associated with eating disorders, but there are four possible mechanisms:
1. Direct Effects on the Brain
Certain infections can directly impact the brain and lead to psychological symptoms that can contribute to eating disorders. For example, patients with toxoplasmosis are more likely to develop OCD or OCD-related tendencies, both of which are common in patients with eating disorders.
2. Inflammation & Autoimmunity
In some cases, the immune response after an infection can result in widespread inflammation and even autoimmunity to the brain, where the body produces antibodies that attack itself. In children with PANDAS, strep antibodies can attack the brain and lead to obsessions, compulsions, and disordered eating.
3. Effect of the microbiome
Antibiotics used to treat infections can decrease the diversity and the number of good bacteria in the gut. Since gut health is connected to brain health, these changes can contribute to changes in emotions and behaviors. For example, decreased gut bacteria and diversity has been linked to obsessive and compulsive behaviors.
4. Appetite suppression
Some infections suppress appetite, similar to when you catch a cold and don’t feel like eating. When this happens, patients may start skipping meals. If they’re praised for losing weight or eating less, this can encourage future disordered eating.
How are eating disorders and PANS & PANDAS related?
Both eating disorders and PANS & PANDAS involve fears around food and unhealthy eating behaviors.
Eating disorders are usually diagnosed in teenage girls and are commonly driven by fears about body image and appearance. PANS & PANDAS are usually diagnosed in young boys during early childhood, and the disordered eating behaviors, when present, are commonly driven by fears about contamination, choking or swallowing, and sensory issues with food.
In one clinical study, researchers found that 52% of children with eating disorders also met the criteria for PANS or PANDAS diagnosis, meaning many patients with eating disorders may have the same immune dysfunction or infectious triggers seen in children with PANS & PANDAS.
You can learn more about PANS & PANDAS in our two-part series.
How do you treat anorexia and other eating disorders?
All patients struggling with eating disorders deserve to have the best chance of recovery, which means considering biological factors in their diagnostic evaluation and treatment.
One study found that about two-thirds of patients hospitalized with an eating disorder were still suffering from their condition 10-20 years after their initial diagnosis. In other words, many patients with eating disorders never fully recover even with current treatments. These grim statistics show us how there needs to be better treatment options for those suffering with eating disorders.
For patients with evidence of inflammation and infections, treating biological root causes can make all the difference in recovery. In my clinical experience, I have seen patients who weren’t responsive to talk therapy become more flexible and willing to change once we took a whole-body approach to treatment.
What does whole-body treatment for eating disorders look like?
In addition to therapy and any necessary medications, patients with eating disorders may also need:
- Nutrition and dietary changes to support gut health
- Treatments that address relevant biological imbalances (ex. inflammation, blood sugar regulation, mineral deficiencies, etc.)
- Testing for infections based on medical history and physical exam, and appropriate treatment when needed
- Ways to manage stress and anxiety (ex. yoga, meditation, biofeedback or neurofeedback)
A New Path for Recovery from Eating Disorders

Since I started recognizing the role of infections in eating disorders and behaviors, some of my patients have improved in ways they never thought would be possible. They have become less fearful, rigid, and more able to benefit from the therapy they were already receiving.
Many patients with eating disorders feel stuck in a cycle. Even those who get better often relapse and need treatment again. I hope that more doctors will recognize and address the biological aspects of this condition so that we can help these patients break out of this pattern and find the path to recovery.
Resources for recovery from eating disorders
If you or someone you care about is suffering from an eating disorder and are interested in the integrative medicine approach, you can visit the following databases to find a practitioner near you:
- Integrative Medicine for Mental Health: The practitioners on this list use an integrative approach, and some have experience or expertise in treating infections and eating disorders.
- PANDAS Network: Many practitioners on this list have experience with diagnostic workups and testing for infections in eating disorders.
References
1. “Eating disorders – Symptoms and Causes” Mayo Clinic
2. “Anorexia Nervosa and the Immune System—A Narrative Review” Journal of Clinical Medicine (2019)
3. “Clinical features of paediatric acute-onset neuropsychiatric syndrome: findings from a case– control study” BJPsych Open (2019)
4. “Anorexia of infection: current prospects” Nutrition (2000)
5. “Disordered Eating and Food Restrictions in Children with PANDAS/PANS” Journal of Child and Adolescent Psychopharmacology (2015)
6. “Association of Exposure to Infections in Childhood With Risk of Eating Disorders in Adolescent Girls” JAMA Psychiatry (2019)
7. “Certain Eating Disorders May Be a Neuropsychiatric Manifestation of PANDAS: Case Report” Journal of the Canadian Academy of Child and Adolescent Psychiatry (2007)
8. “Infection and anorexia” The Turkish Journal of Pediatrics (2006)
9. “The Gut Microbiome in Anorexia Nervosa: Friend or Foe?” Frontiers in Psychiatry (2021)
10. “Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden” Current Opinion in Psychiatry (2020)
11. “Eating Disorders: Core Interventions in the Treatment and Management of Anorexia Nervosa, Bulimia Nervosa and Related Eating Disorders” British Psychological Society (2004)
The information and any products mentioned in this article are not intended to diagnose, treat, cure, or prevent any disease. The information provided is for educational purposes only and not intended to replace the relationships with your physician(s). Before initiating any conventional or integrative treatments, please first consult with a licensed medical provider. Please review references cited at the end of article for scientific support of any claims made.
Suruchi Chandra, MD
By
June 7, 2021
|







