Persistent or chronic depression can be extremely frustrating to live with, especially if you’ve tried multiple treatments with few results. A recent survey found that even with talk therapy and medications, only 46% of patients experience full remission of their symptoms.
However, new advances in neuroscience have changed our understanding of the brain and opened up roads to new treatment options. One promising therapy is transcranial stimulation, which uses gentle electric currents to lift people out of depression. These currents in transcranial stimulation support the brain’s natural electrical wiring and encourage healthier brain activity for better functioning.
In this article, we discuss the science and research behind transcranial stimulation, including questions such as:
- What is transcranial stimulation?
- How does transcranial stimulation help with depression?
- Does transcranial stimulation therapy work? Is it effective?
- What other conditions can transcranial stimulation be helpful for?
- Is it safe? What are the side-effects?
- Will the results last?
What is transcranial stimulation?
Transcranial stimulation is a gentle, non-invasive form of brain stimulation. It involves placing two or more electrodes on the scalp and running a very low level of current through them. No surgery or anesthesia is needed for the session, and patients can resume their day as normal after treatment.
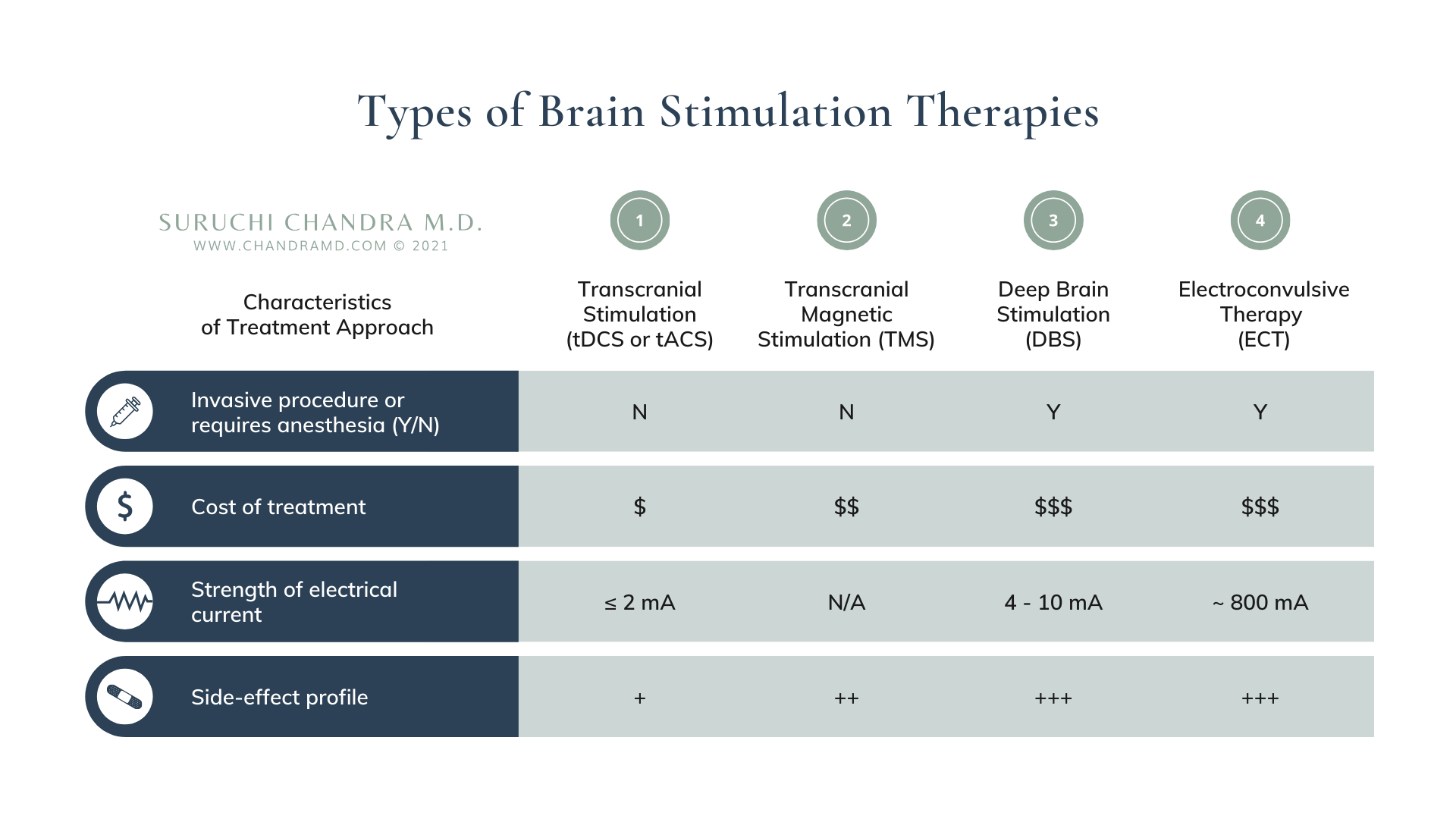
Many people are understandably intimidated by the idea of putting electrical current into the brain. However, the current used in transcranial stimulation is 400 times more gentle than the current used in electroconvulsive therapy (ECT), and is generally well-tolerated and safe.
Finally, there are three different types of transcranial stimulation, with direct current stimulation (tDCS) being the most popular, followed by alternating current (tACS) and random noise stimulation (tRNS).
What is the difference between tdcs and tms?
You may be wondering how tDCS differs from TMS, or transcranial magnetic stimulation, which is currently the best-known form of brain stimulation for depression.
TMS uses electromagnetic coils that stimulate brain cells and cause them to “fire,” or activate. On the other hand, the low-level electrical current used in tDCS does not force brain cells to fire, but rather gently encourages them. This means that while TMS may have more powerful effects, it may also result in more side-effects. More differences between TMS and tDCS include:
Transcranial Direct Current Stimulation (TDCS)
- Still considered investigational by the FDA
- Usually not covered by insurance
- tDCS devices are more portable and affordable
- Available for home-use
- May be individualized to patient’s specific needs in clinics
Transcranial magnetic stimulation (TMS)
- Has been FDA-approved for certain devices and conditions
- May be covered by insurance
- TMS devices are quite large and more costly
- Not available for home-use
- Typically protocol-based in clinics
Currently, we do not have enough comparative studies to determine whether TMS or tDCS is more effective, but some preliminary reviews have found them to be similarly effective for depression.
Even though we do not have conclusive evidence yet, transcranial stimulation deserves more attention from clinicians and researchers because of its accessibility and ability to help more people than any other form of brain stimulation.
How does transcranial stimulation help with depression?
To understand how transcranial stimulation works, it’s helpful to first look at the brain’s biology.
For example, the prefrontal cortex (i.e. the very front of the brain located behind the forehead) is involved in planning, decision-making, and emotional regulation. However, in patients with depression, imaging technology often shows slower-than-normal brain wave activity in this area. This means that in depression, slow activity in the prefrontal cortex can contribute to feeling sluggish, unmotivated, and sad.
Most transcranial stimulation protocols for depression involve placing an electrode over the left prefrontal cortex to stimulate or boost activity in this area. This type of therapy is like exercise for your brain and may have broad benefits like increased blood flow and reduced inflammation. tACS, or alternating current stimulation, can also encourage faster and healthier patterns of brain wave activity in the prefrontal cortex.
Does transcranial stimulation work? Is it effective?
Recently, there have been many promising studies about transcranial stimulation for depression. One survey or meta-analysis of the current research found comparable effects between tDCS, TMS, and antidepressant medications for major depressive episodes.
However, not all studies have come to the same conclusion. There are many possible reasons for this inconsistency. For example, there are no standard protocols for transcranial stimulation, and studies may vary in the number of sessions, power of electrical current, type of current, and more.
Before we can answer how effective transcranial stimulation really is, clinicians and researchers need to understand how to best use it.
Improving outcomes with transcranial stimulation
There are two main ways that we can improve our understanding of transcranial stimulation:
1. Determine what type of transcranial stimulation is most effective. There are three types of transcranial stimulation that differ based on the type of current used:
- Transcranial direct current stimulation (tDCS). tDCS uses a constant current that runs in the same direction between electrodes.
- Transcranial alternating current stimulation (tACS). tACS uses a current that goes back and forth between the two electrodes at a set rate or frequency. This current creates a waveform that can mimic and encourage healthy brain function.
- Transcranial random noise stimulation (tRNS). Random noise is a current that goes back and forth at a random frequency and power between two electrodes. Some clinicians and researchers are using pink noise to improve treatment protocols.
Most of the research in the field has been focused on tDCS, in part because it is easier to implement. However, some studies show that tACS or random noise may be equally or even more effective.
2. Determine which part of the brain to target during treatment. Not everyone with the same diagnosis has the same brain activity. For example, not everyone with depression has the same slow activity in the prefrontal cortex. This means that different patients may require different treatment protocols or electrode placement.
As we improve our transcranial stimulation techniques as a field, research may also provide us with a better understanding of how this treatment can help those with brain-based conditions.
Is transcranial stimulation FDA approved?
Based on the positive research data, tDCS has been approved for depression in the European Union. It is still considered experimental in the U.S., but some biotech companies have received FDA approval to conduct clinical trials of tDCS for depression (1, 2).
Given the promising research and its positive safety profile, some academic centers and clinics have already started using transcranial stimulation, including Johns Hopkins University, New York University, and Mount Sinai Hospital.
The takeaway: Early studies have found promising benefits of transcranial stimulation for depression. More research is needed to determine the best type of stimulation (direct, alternating, or random current) and the most effective treatment protocols.
While it is not FDA approved yet, some academic centers and hospitals have already started incorporating tDCS as part of their treatment protocols for brain-based conditions because there is a great need for treatments that are affordable and effective.
What else can transcranial stimulation be used for?
Because transcranial stimulation can have broader effects in the brain (ex. reducing inflammation, increasing blood flow), it may be useful for a wide array of brain-based conditions, such as:
- OCD
- ADHD
- Stroke or traumatic brain injury
- Movement disorders
- Cognitive decline
- Language or communication disorders
However, we need much more research before we can conclusively determine if transcranial stimulation is effective for these conditions.
Our Clinic’s Experience with Transcranial Stimulation

In addition to improvement of their depression, our patients have reported better focus, cognitive processing, ability to learn, and sleep quality after transcranial stimulation. Based on the positive feedback from our patients, we use transcranial stimulation as an important part of our treatment approach for many brain-based conditions.
We have recently incorporated random noise into our tDCS and tACS treatment protocols in an effort to improve patient outcomes. We also use qEEG brain mapping techniques to visualize a patient’s unique brain function and tailor treatment to their specific needs.
After their transcranial stimulation sessions, patients in our practice often describe feeling “lighter” or a “lifting” of their depression. Patients have also reported:
“Since starting neurostim treatment, I’ve noticed that I can be more present for experiences in my life.”
“I’ve had noticeably deeper sleep.”
“Transcranial stimulation therapy has helped me become more resilient, allowing me to manage stress better.”
Is transcranial stimulation safe? Are there side-effects?
Transcranial stimulation is the gentlest and safest form of brain stimulation currently available. In a review of over 180,000 patient sessions, there were no serious side-effects or signs of irreversible tissue injury. Due to its positive safety profile, the European Union has even approved transcranial stimulation for home use.
If side-effects occur, they are usually mild and localized to the site of the electrodes. The most common side-effects include mild discomfort, itching, or skin irritation under the electrode site during a session, and usually go away once the electrodes are removed.
Very rarely, patients report headache or fatigue immediately after the session. These are generally mild and short-lived, and can often be managed by adjusting the settings of the treatment.
Will the results of transcranial stimulation therapy last?
Transcranial stimulation can create both immediate and long-lasting changes in the brain, just like exercise can for the body.
During a session, patients may feel a lifting of their mood and a sense of relief or focus that they didn’t have before. Even after the session ends, the brain may continue to rewire and heal itself thanks to its neuroplasticity, or its natural ability to change. Patients may be able to consolidate gains with repeated sessions, and clinicians can visualize long-term changes in the brain with imaging techniques (i.e. fMRI or qEEG).
While the potential to create lasting change in the brain is promising, current research does not conclusively state the extent of these changes or how long they may last. Results may vary based on the number of sessions, type of current used, power, severity of condition, and more.
Brain Stimulation: The Future of Psychiatry
The newest discoveries in neuroscience have taught us that the brain is a complex computational system with intricate networks. In the future, more doctors will administer treatment not just in capsules or tablets, but also through waveforms: sound, light, and electrical current.
Transcranial stimulation is a promising new tool that builds on these innovations in science and offers hope to those struggling with depression. In the end, however, it may not address the complex root causes of depression, such as inflammation, gut microbiome imbalances, and more. Transcranial stimulation may be best used as a helpful tool in a comprehensive approach to give patients the best chance at long-term, sustainable healing.
References
1. “Low-Intensity Transcranial Current Stimulation in Psychiatry” – The American Journal of Psychiatry (2017), DOI: 10.1176/appi.ajp.2017.16090996
2. “Lasting connectivity increase and anxiety reduction via transcranial alternating current stimulation” – Social Cognitive and Affective Neuroscience (2018), DOI: 10.1093/scan/nsy096
3. “Transcranial alternating current stimulation (tACS): from basic mechanisms towards first applications in psychiatry” – European Archives of Psychiatry and Clinical Neuroscience (2020), DOI: 10.1007/s00406-020-01209-9
4. “Transcranial Alternating Current Stimulation (tACS) Mechanisms and Protocols” – Frontiers in Cellular Neuroscience (2017), DOI: 10.3389/fncel.2017.00214
5. “Noninvasive brain stimulation with low-intensity electrical currents: putative mechanisms of action for direct and alternating current stimulation” – The Neuroscientist (2009), DOI: 10.1177/1073858409336227
6. “Boosting the LTP-like plasticity effect of intermittent theta-burst stimulation using gamma transcranial alternating current stimulation” – Brain Stimulation (2018), DOI: 10.1016/j.brs.2018.03.015
7. “Transcranial Alternating Current Stimulation (tACS) as a Tool to Modulate P300 Amplitude in Attention Deficit Hyperactivity Disorder (ADHD): Preliminary Findings” – Brain Topography (2020), DOI: 10.1007/s10548-020-00752-x
8. “Effects of weak transcranial alternating current stimulation on brain activity—a review of known mechanisms from animal studies” – Frontiers in Human Neuroscience (2013), DOI: 10.3389/fnhum.2013.00687
9. “Comparison of Three Non-Invasive Transcranial Electrical Stimulation Methods for Increasing Cortical Excitability” – Frontiers in Human Neuroscience (2016), DOI: 10.3389/fnhum.2016.00668
10. “An experimental depression treatment uses electric currents to bring relief” – NPR (2022)
The information and any products mentioned in this article are not intended to diagnose, treat, cure, or prevent any disease. The information provided is for educational purposes only and not intended to replace the relationships with your physician(s). Before initiating any conventional or integrative treatments, please first consult with a licensed medical provider. Please review references cited at the end of article for scientific support of any claims made.
Suruchi Chandra, MD
By
April 13, 2022
|






